UnitedHealthcare is facing federal fines for creating misleading ads to promote its Medicare Advantage plans.
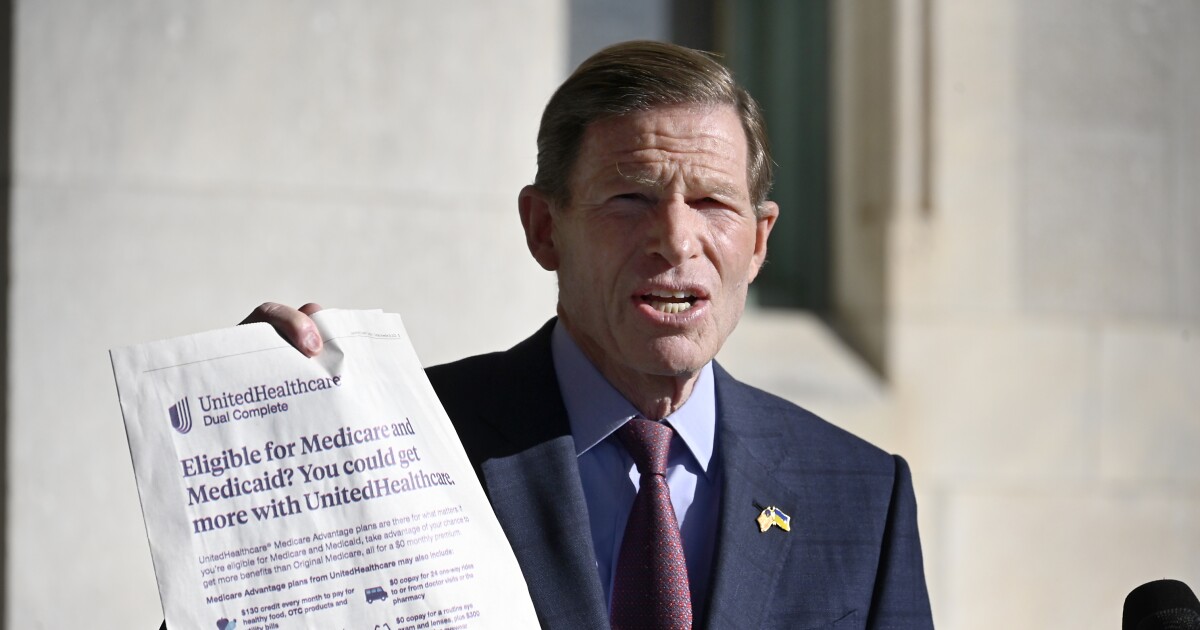
Democratic Senator Richard Blumenthal said ads targeted at seniors, low-income people and people with disabilities promise extra benefits but actually limit their access to health care.
“UnitedHealthcare lured thousands of Connecticut patients with this deceptive and misleading advertising,” Blumenthal said.
Advertisements placed in local newspapers around the state promised applicants additional benefits not included in regular Medicaid or Medicare plans.
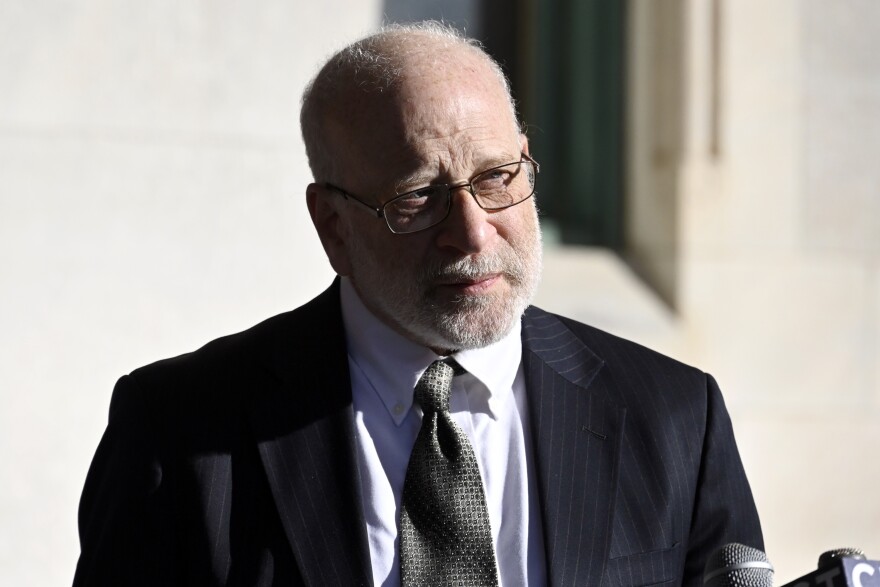
Speaking at the State Capitol in Hartford on Tuesday with Sheldon Taubman, a litigation attorney with the Connecticut Disability Rights Organization, Blumenthal said 94,000 people statewide in 2023 are enrolled in plans that limit in-network providers and add red tape requirements.
Not only are they arguing for government intervention, but they also want the companies to allow people to opt out of the plans.
Blumenthal said the plan’s drawbacks outweigh its benefits.
“They’re going to be like, ‘Oh, we don’t do Medicare Advantage, so sorry, you’re going to have to see a new doctor,'” Blumenthal said.
Taubman said the group focuses on representing adults who are eligible for both Medicare and Medicaid, known as dual eligibles.
Eddie Martinez
/
Connecticut Public
Disability rights group Connecticut attorney Sheldon Tubman and Sen. Richard Blumenthal speak at the State Capitol on Tuesday, Jan. 2, 2023. Blumenthal and Tubman allege that UnitedHealthcare misled applicants into signing up for Medicare Advantage by claiming the plan offered supplemental benefits. They now say the plan actually limited access to care, and Blumenthal is now calling for a federal investigation of the provider.
He gave the example of dental and vision coverage: Traditional Medicare and Medicaid don’t cover many routine dental procedures, such as fillings and dentures.
The plans, which advertised they offered dental coverage, failed to include potential risks associated with enrolling in the plans, such as additional barriers to approval for treatment, he said.
“Maybe we should tell them that if they have Medicare Advantage, there are limited prior authorizations that apply,” Taubman said.
UnitedHealthcare denied the allegations in a statement.
“These allegations are completely without merit,” UnitedHealthcare said in a statement. “All UnitedHealthcare DSNP plans in Connecticut allow members to see any provider that accepts Medicare and offer benefits that are superior to Medicaid alone, including dental and vision enhancements, monthly health supplements, OTC and utility credits. Our plan benefits are applied for and approved by CMS, and our advertising factually describes these benefits and is applied for in accordance with CMS guidance.”
Medicaid provides additional assistance to income-limited adults, but dental care is only covered for children and dual-plan enrollees must pay out of pocket.Medicare Advantage essentially functions as supplemental insurance run by private companies.
Blumenthal and Taubman are not alone: The American Hospital Association recently published a letter calling on the Medicare Payment Advisory Commission (MedPAC) to collect data on Medicare Advantage denials.
The letter also cited a 2022 Department of Health and Human Services study that showed Medicare Advantage plan enrollees had higher denial rates than regular Medicare plan enrollees.
Blumenthal called on the government to fine the company, but also called on UnitedHealthcare to take appropriate action for the 94,000 people who enrolled in the plan.
“That’s what we’re asking for, and retroactively, that people who have been taken off of traditional Medicare and Medicaid plans be given the option to get back in.”